Chimeric Antigen Receptor T-cell therapy, also known as CAR T-cell therapy, is a form of immunotherapy that has shown great promise in treating certain types of blood cancers. CAR T-cell therapy uses a personalized approach to target and destroy cancer cells using the patient’s own immune system.
CAR T-cell therapy has emerged as a promising treatment option for a range of blood cancers. It utilizes genetically modified T cells to help target and eliminate cancer cells. CAR-T cell therapy has expanded and offers new hope for patients with previously limited treatment options.
CAR T-cell therapy is an example of how immunotherapy is transforming cancer treatment
The process of CAR T-cell therapy
CAR T-cell therapies are personalized for each patient. They are made by obtaining the patient’s T cells and recreating them in a specialized laboratory through an intricate process that can take several weeks.
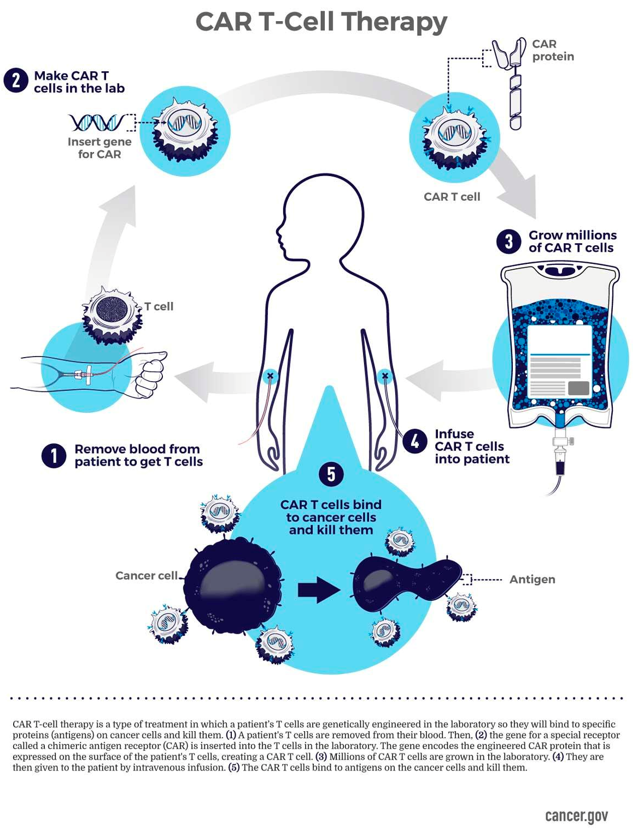
NIH. National Cancer Institute. CAR T-Cell Therapy Infographic
Cell collection
Patient’s blood is drawn, and T cells are collected, removed, and separated from the blood.
Cell creation
CAR T-cells are created in a special laboratory through a process. CAR genes are inserted into the T cells. Millions of CAR T-cells are produced.
Cell infusion
CAR T-cells are returned to the patient’s bloodstream via IV infusion in a hospital or clinic.
Cell activation
The CAR T-cells circulate in the bloodstream, attaching to the cancer cells and killing them.
Cell expansion
The CAR T-cells can continue to multiply which helps provide long-term activity of these cells with the goal of preventing cancer relapse.
Learn more about this process here.
Which blood cancers are available for CAR T-cell therapy?
The field of CAR T-cell therapy is rapidly evolving. Ongoing research is expanding its use to include additional blood cancers and solid tumors. CAR T-cell therapy provides viable treatment options for patients who may not have many options left.
Patients with blood cancers should discuss treatment options and eligibility for CAR T-cell therapy with their healthcare team to determine the most appropriate course of action based on individual patient factors.
CAR T-cell therapy can help treat the following blood cancers:
- B-cell Acute Lymphoblastic Leukemia (ALL)
- B-cell Non-Hodgkin Lymphoma (NHL)
- Diffuse Large B-cell Lymphoma (DLBCL)
- Primary Mediastinal B-cell Lymphoma (PMBCL)
- Follicular Lymphoma (FL)
- Mantle Cell Lymphoma (MCL)
- Diffuse Large B-cell Lymphoma (DLBCL)
- Multiple Myeloma (MM
These treatments are typically appropriate in patients who have tried and failed other treatment options. Consider discussing with your provider if CAR T-cell therapy may be an option for you.
Hope for the future
CAR T-cell therapy continues to develop with ongoing research aiming to improve its safety and effectiveness. For patients facing challenging blood cancers, CAR T-cell therapy represents a treatment option that offers hope for remission and improved quality of life.
– – –
References
- National Cancer Institute. CAR T Cells: Engineering Patients’ Immune Cells to Treat Their Cancers
- American Cancer Society. CAR T-cell Therapy and Its Side Effects